Vitrectomy
Vitrectomy refers to the surgical removal of the vitreous gel at the back of the eye.
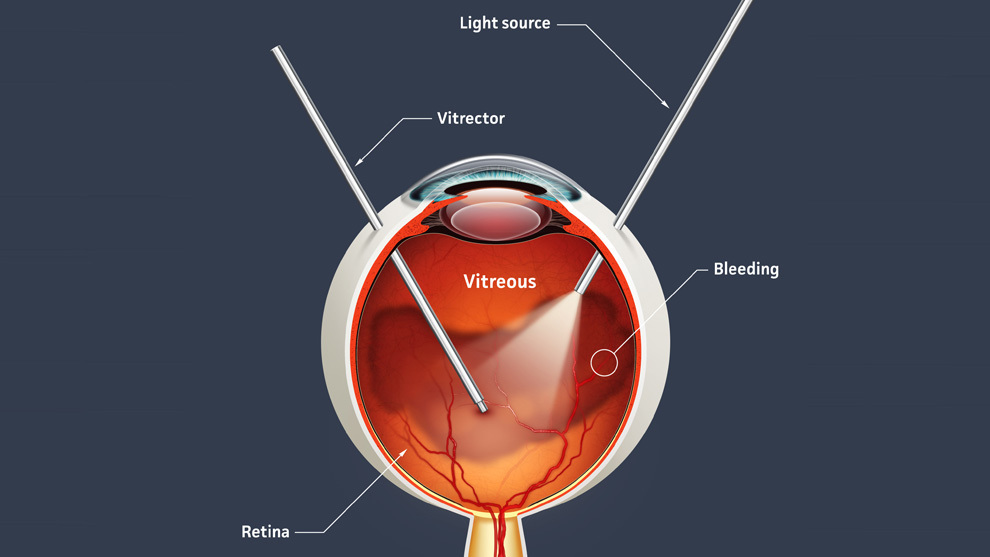
The technology has advanced dramatically since first invented in the 1970s, and now involves ultrafine instrumentation, together with highly advanced vitrectomy machines that closely monitor and stabilise the eye during surgery, enhancing safety and improving surgical results.
Typically, the surgery is performed normally under local anaesthetic, with an injection next to the eye, as this facilitates prompt recovery and reduces any risk from general anaesthesia.
For some patients, general anaesthesia is the preferred option, and this will be discussed with the surgical team prior to listing for surgery.
Surgery for most cases typically takes less than an hour, the eye numbed from the anaesthetic, and apart from a mild pressure sensation around the eye, the procedure is painless. Sometimes the patient can see light and shadows during the procedure, but clear details of the procedure are not visible to the patient.
Recovery is generally rapid, often with no sutures being needed, although sometimes these are necessary, and you will be informed by your surgeon if this is the case.
For some procedures, a medical gas or silicone oil bubble are introduced into the eye at the end of the procedure (please see condition specific information pages for details of this). This can temporarily blur the vision, and your surgeon will give you more details if either of these have been used.
Risks of surgery
Although modern vitrectomy is extremely safe, all surgery on the inside of the eye carries small, but significant risks. These will be outlined to you by your surgeon.
Risks include:
- Infection (< 1:3000)
- Retinal detachment (1:100)
- Bleeding inside the eye (more common with certain conditions, especially diabetic eye disease)
- High or low eye pressure
- Cataract (cataract development is often accelerated after vitrectomy surgery, especially if gas or oil are used. In some cases, cataract surgery is undertaken at the time of vitrectomy. Your surgeon will discuss this with you, if this is appropriate in your case)
- Prolonged inflammation
- Inflammation of the macula (cystoid macular oedema) (1:100)
The vast majority of complications can be easily and effectively managed, with low ultimate risk to vision if picked up early. The most serious risk is an infection, which can irreversibly affect vision, even if treated promptly, but this is extremely uncommon.





