Retinal Detachment
Retinal detachment occurs when the light-sensitive layer (retina) comes away from the lining of the back of the eye.
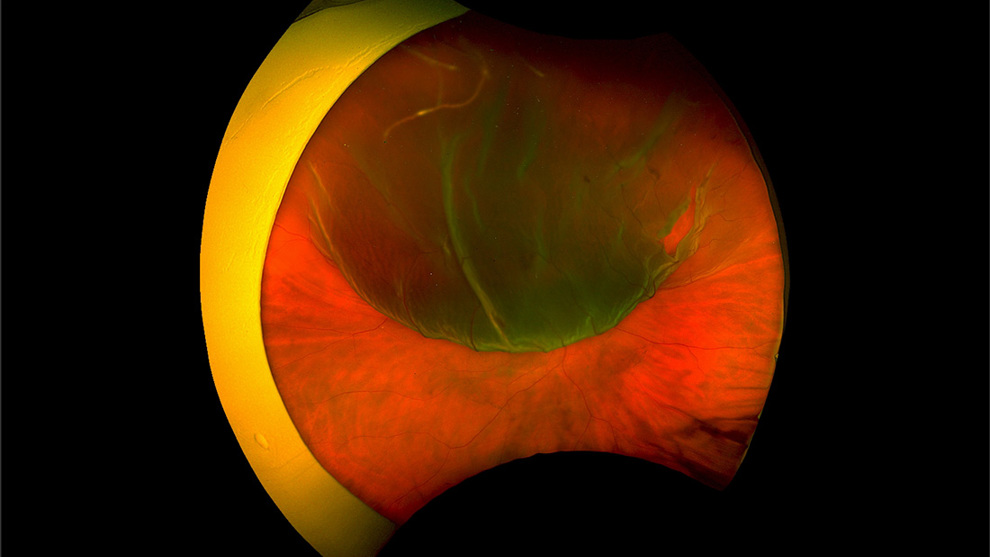
When this happens, the area of the retina that is detached fails to work normally, and often the patient is aware of a shadow in the field of vision. Because light falling on the retina at the back of the eye is reversed when it travels through the lens, the shadow appears in the opposite field of view for the patient. For instance, if the retina at the top of the eye starts to detach, the shadow appears in the lower (reading) part of the visual field for the patient.
This explains why in some cases, patients are unaware of the detaching retina until much of the retina has detached, if the lower part of the retina is involved; in which case there may already be a significant amount of damage to the retina when the patient presents.
Most retinal detachments can be repaired, and if caught early, can still result in a good visual outcome.
Usually, the detachment is caused by a small tear that develops in the retina due to changes in the vitreous gel at the back of the eye that occurs with age.
Everyone at some point will experience floaters, or small dots in the vision, and in many cases, these are completely normal. A sudden increase in very noticeable floaters can indicate a sudden change in the gel at the back of the eye, which in a small number of patients can signal a tear in the retina, with or without the beginnings of a retinal detachment.
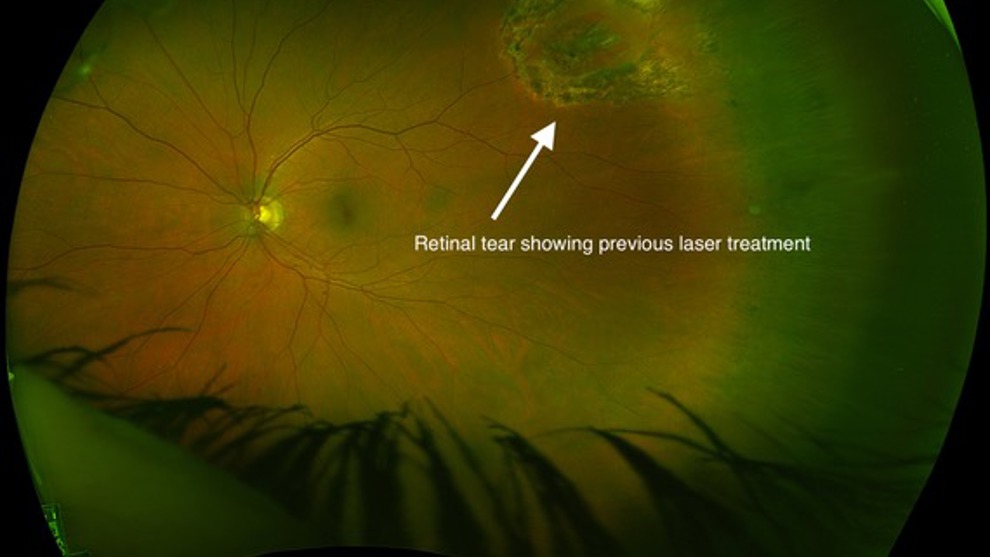
Tears in the retina can often be caught early in some cases before the retina has started to come away. These may be picked up by your optician or when you attend the eye clinic. If caught early, the tear can often be treated with some simple laser treatment in the eye clinic.
For patients in whom an operation is necessary to repair the retina, there are several possible different approaches, and your surgeon will discuss these with you. Often, the type of approach will depend on your age and the type / cause of your detachment.
Most patients will require an internal approach that involves a procedure called a vitrectomy. During this procedure, which is usually performed under local anaesthetic as a daycase, tiny instruments are inserted into the vitreous cavity of the eye and the gel is removed before a bubble of gas or a medical oil (silicone oil) is injected to reattach the retina whilst treating the tear in the retina with laser or freezing therapy (cryotherapy).
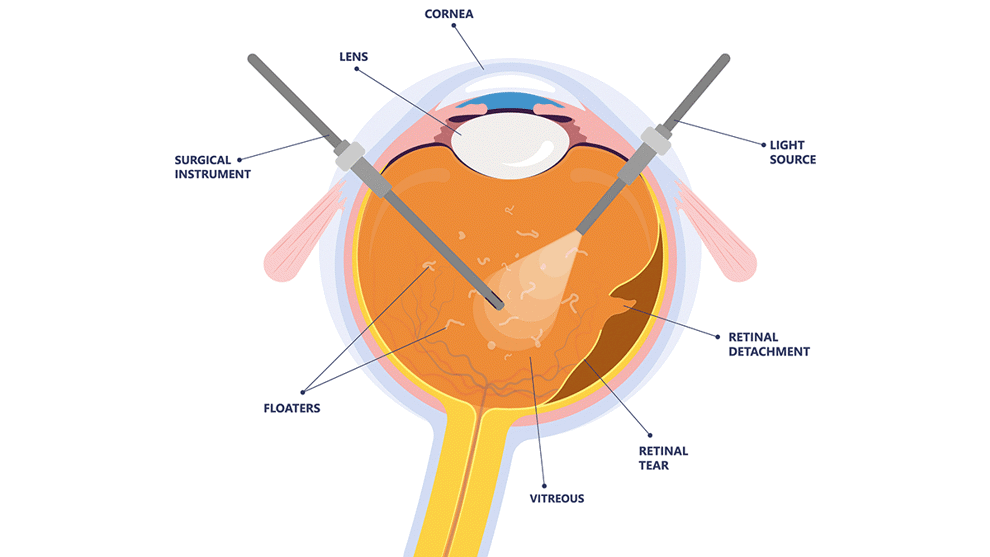
The gas or oil bubble will temporarily blur the vision for a period of time. The gas will dissipate over 2 – 8 weeks depending on the type of gas used, whereas if silicone oil is used, this will stay inside the eye until it is removed at a later date, when the retina is stable. The choice of gas and whether or not oil is used depend on a number of factors, and your surgeon will explain these to you.
After the surgery, you may be asked to position in a certain way to optimise the contact of the gas or oil with the retina and increase the chances of successful reattachment. Avoiding work or strenuous activity for 2 weeks is standard advice, but varies from patient to patient and depends on the specifics of the procedure to some extent. Your surgeon will give you clear advice in relation to this.
In approximately 80% of patients, the retina reattaches after one procedure, but in 10-15% of patients, further surgery may be required to fully reattach the retina. In 1-5% of patients, for various reasons, the retina fails to reattach.
As with any operation on the inside of the eye, there are small risks of bleeding and infection, with the risk of infection being less than 1:3000.
For patients who have not previously undergone cataract surgery, development of a cataract is almost universal after the procedure. This is easily dealt with following the repair of the retina.
In many cases, vision is restored to the level it was before the detachment. There may be slightly duller vision in the field of vision affected by the retinal detachment, and this may be permanent, as the retina is highly sensitive tissue that is usually irreversibly affected by a period of detachment.
Where the detachment involves the central vision (macula) unfortunately the vision is likely to permanently affected.





