Diabetic Eye Disease
Diabetes is a common condition. With time, it can affect many parts of the body and careful management of blood glucose and other health parameters can help to reduce the risk of developing complications.
Patients diagnosed with the condition will have regular eye screening undertaken by the Diabetic Retinal Screening program.
Patients can develop several complications in relation to their eyes, and these are usually picked up through photographic screening, and subsequent referral to the eye department for further management.
Diabetic macular oedema is the most common complication, where blood vessels in the macular area leak fluid and cause blurred or distorted central vision.
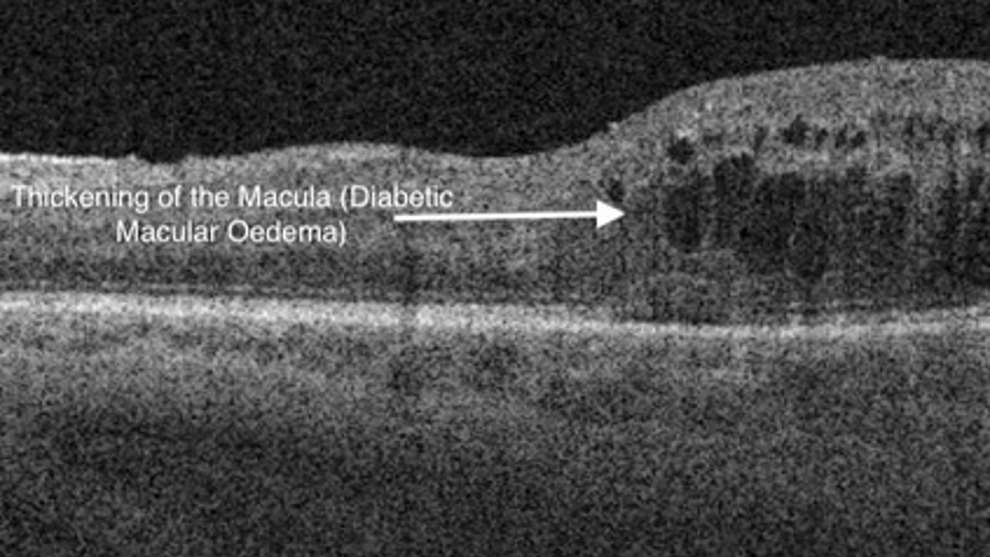
This can be treated with laser treatment as an outpatient, or in more severe cases, injection of drugs known as anti-VEGF agents, into the eye as a course of injections.
Some patients develop abnormal blood vessels at the back of the eye, as a response to the damage caused by high blood glucose levels. These blood vessels are an attempt by the eye itself to repair some of the damage, but unfortunately the vessels are very delicate and are prone to bleeding spontaneously.
Such blood vessel growth can be prevented and reduced by laser treatment as an outpatient, known as panretinal photocoagulation (PRP), which targets the damaged retina around the periphery of the eye. The peripheral field of vision can eventually be affected by this treatment, but the aim is to protect the central vision.
Where bleeding occurs, this can be very damaging to the eye, as it can lead to scar tissue formation over the retina, and ultimately, detached retina and loss of vision if unchecked.
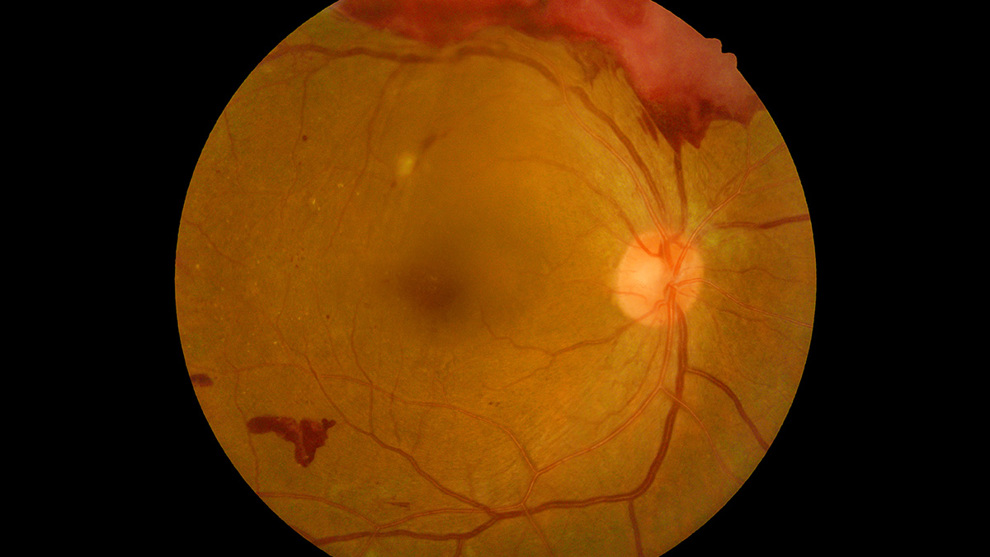
Prompt laser treatment can prevent this complication, but where it does occur, vitrectomy surgery is often necessary to clear the blood and stabilise the retina to protect vision.
The surgery is usually performed under local anaesthetic as a daycase. The vitreous gel at the back of the eye is removed using tiny instruments and at the same time, the blood is cleared and any scar tissue is removed from the retinal surface. Usually, further laser will be applied at the time of surgery.
In some cases, a medical gas bubble is inserted into the eye to stabilise the retina at the end of the procedure. This will blur the vision temporarily, but will gradually dissipate by itself. Occasionally, a medical oil (silicone oil) is used for longer-term stability, especially if the diabetic damage is more advanced. When this is used, the oil is usually removed via a second procedure at a later date. Your surgeon will keep you updated during / after your surgery as to which method is used.
Aftercare
With modern vitrectomy surgery, the eye generally heals fairly rapidly, with minimal discomfort. Occasionally there is some mild irritation, especially if sutures are used, but your surgeon will inform you if this is the case.
You will be prescribed eye drops post-surgery, and it is important you follow the relevant directions.
It is important that you avoid getting water directly into the eye for the first week after surgery, and swimming needs to be avoided for up to 3 months.
With gas inside the eye, it also means that you cannot fly in an aircraft, dive, or ascend to very high altitude, due to the effect of atmospheric pressure on the size of the gas bubble. Dangerous, sight-threatening rises in eye pressure can occur in these situations.
Normally patients are reviewed approximately at 2 weeks and then 2 months after the procedure to ensure everything is settling well.
If there are any unexpected symptoms, in particular increasing pain or dramatic drop in vision, or you have any other postoperative concerns, it is very important that you contact your surgeon. Emergency contact details will be provided upon discharge from the hospital.
Risks of surgery
Please follow this link for the risks associated with vitrectomy surgery.





